Danish Bhatti: Welcome John. It is another episode of Movement Disorder podcast where you share the stories that the patients have taught you, with us. What story would you like to share with our listeners today.
John Bertoni: Well I think we can call this one Paying Attention to Details.
Danish Bhatti: Paying attention to details. That’s interesting. So tell us the background of this story. Where were you when this episode happened, in what setting and what was going on around that time.
John Bertoni: Every so often, we have to renew our skills in CPR and there’s basic CPR and now we call life support. So it was my turn. I was at the V.A. (veterans administration hospital) I figured it’d be easy at the V.A. because is not a big line over there.
Danish Bhatti: So V.A. is a Veterans Administration hospital.
John Bertoni: Right.
Danish Bhatti: And the CPR will be the Cardiopulmonary resuscitation of basic life support.
John Bertoni: Yes.
Danish Bhatti: And where were you in your career?
John Bertoni: This was so 5 years ago maybe a little longer.
Danish Bhatti: When you were full professor and chair of Department.
John Bertoni: This was actually it was when I was over here at UNMC (university of Nebraska Medical Center). So let’s say 5 to 7 years ago I know because I recently had come back from a trip to Africa. So I’d have to. But anyway let’s say 5 years ago. So there was a written test (for Basic Life Support (BLS)) and back then it wasn’t online. So I had something to fill out or I had completed that right. Came in for the practical and there was a lady maybe late 30s, overweight, happened to be black. Very nice. And I explained to her I just passed the written exam and she stood up and walked over to get the dummy, the mannequin. It was just the upper half. So from the waist up whatever resucci-annie, I dont know what the guy’s name Resucci-Andrew.
Danish Bhatti: So a mannequin to practice just to practice chest compression and
John Bertoni: Right and then breathing. Yeah. So and then you have to make sure that you’re putting enough air in the chest has to be elevated and that can’t be your leakage in all that. So but I was noticing standing up was slow and (for her) for her for somebody in her 30s. OK. I’m thinking I can’t ever stop being a doctor and I go out with my wife and we’re walking down the street and I say this guy has a foot drop See Notice how you know where he has a gluteus medius weakness you can see the way he walks and she tries to get me to relax and just be a regular person but I can’t help it. So I noticed this and then I noticed that she went and picked up the mannequin and put it on the table between us and then she was short of breath. So I passed this course. But before I did so I just said you’re short of breath. And she said Yeah I’ve been short of breath for a few weeks now and she had in her hand a plastic cup like the one on your desk and I looked and it had ice in it. So I said How long have you been eating ice. So again you can see the gears turning in my head. And now I’m the doctor again and she’s evaluating me, but nobody’s asked these questions.
Danish Bhatti: She’s your trainer for the day and evaluator.
John Bertoni: Mm hmm. So then the question is how long have you been chewing ice. She says only for the past couple of weeks. So then the question is if there’s anybody out in airwave land who’s listening in. What’s the next question to ask. I can see where I’m going with this. Because she shouldn’t be so short of breath and eating ice in OK. Ice is a non dietary thing to be chewing. People do it. It’s called pica – eating a non-food item and people will chew on clay in the ground or chew on almost anything pencils anything.
Danish Bhatti: But chewing on the clay we attribute it to an iron deficiency in evolutionary response and humans do eat maybe clay which may be rich and high iron (that might have iron in it) like the orange mud (sure) that you see.
John Bertoni: Right there is and I think the fact that you’re eating. I think there is an evolutionary advantage that we have when we get iron deficient we start eating non-food items and ice isn’t going to do anything for you. But people will put almost anything in their mouth. One of my colleagues where I worked before said there was a woman who used to reach up and break off a little dry wall and then bring a piece of it and start chewing it.
Danish Bhatti: is the paint, is the painting …..
John Bertoni: No no it’s actually it’s behind the paint. It’s the oh like 3/8 inch or half inch.
Danish Bhatti: Is there some metal in the wall.
John Bertoni: No I think it’s made out of gypsum or something. It’s earthy substance anyway. So people chew on nails some people actually will put nails into an apple and let it rust and then eat the apple which does have iron in it obviously. But I don’t know if that’s a remedy or something that they’ve learned to do. So the next question. There are many other questions that you can ask at this point. So I just went right straight toward the jugular here and said if you ever had any anemias (lack of blood) and she said oh yeah when I had my right after my first child or whatever I had to take iron supplements and I said Well how do they manage that. And so it took a while but she eventually got over that and then she had nothing major recently that she could think of but she was very short of breath and she said she wasn’t feeling right and she didn’t have a lot of money. So I said Can I see your hand.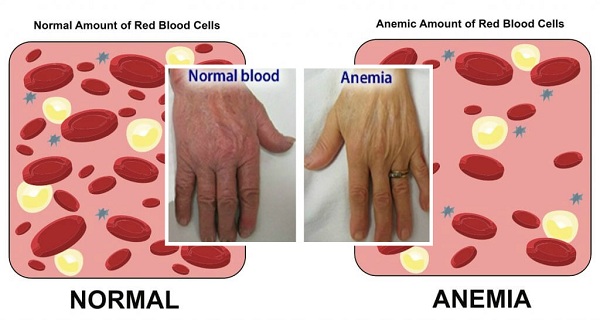
Danish Bhatti: Is it because she works the V.A.
John Bertoni: I don’t know. I mean I don’t think the V.A. is paying her a lot. The V.A. doesn’t pay one of their own employees to do this. So she’s probably not getting benefits and I don’t know whether she had health insurance. So I looked at her hand in his you know the creases in your palm are a giveaway because if you don’t have pigment there you’re probably six grams of hemoglobin or less. I don’t know what the cutoff was and I said you are seriously anemic. And I said you have to go see somebody. So then what’s the next idea that comes in your head. I’m at a hospital right. So the next question at the V.A. hospital is are you a veteran. No she’s never served in the military. You know she’s never had to and never did. So then what do you do. Just say well you got to go get this taken care of.
Danish Bhatti: That’s when most people will start to say goes to your regular doctor. Go an emergency. You think she’s that bad. She needs to go to an emergency to have bloodshed.
John Bertoni: Well here it was bad enough that I said OK I know somebody that I met on a trip to Africa.
Danish Bhatti: Just a short while before this happened.
John Bertoni: Just a short while maybe a month maybe six months to a year. anyway so I’m not going to name his name. He had a private practice and it was known for getting right to the point he actually was a football player for Stanford University. Years and years ago behind a very famous quarterback he was second string and hardly ever got to play. But he was an athlete at one time. You wouldn’t know it. You know as people get older you can’t tell who the athlete was. So I just called him up right then and I said let’s call him Jack. This is John you remember me. And he said Oh yeah yeah. So I said I got a patient for you. Can you see here today. And he said sure what’s the story and I explained and he knew exactly what I was worried about. And I said OK. Give me your phone number and your address and e hand the phone to his assistant. He went back to seeing 20 patients an hour or whatever he was doing. So then I said here’s the phone number here’s the address you know and I gave her the card like one of these and then I did the test and passed it. They might have had a child mannequin there too. But nowadays it’s really way into details that are getting beyond. But anyway now there are mannequins that will tell you’re not blowing fast enough that you can work on and I think that’s not a bad thing. Am I talking too long.
Danish Bhatti: So whatever happened to that lady.
John Bertoni: I didn’t hear. So weeks went by and I asked whatever who was that person and people didn’t. She was a hired gun to come in (temporary) or something like that. So something that was some sort of a deal with you know I contracted employee. So then I got a call out of the blue one night one evening and she said she gave me your name I didn’t remember her name .So I said do you remember me and I saw.
Danish Bhatti: She traced your number.
 John Bertoni: She called me back and I said wow this I was wondering what happened. And she said thank you I think you saved my life and I said what. she said he admitted me. Her hemoglobin was so low she had to get a transfusion night. So I’m thinking well you know how it is if you gradually get more and more anemic and you learn to adapt to it. But if you go from you know a normal hemoglobin to where she was you know you wouldn’t be able to handle it right away. So she was very grateful and I said were there ever figure out why you lost blood and they had done a workup and figured that out. Nothing major league. And I said Well I do appreciate the feedback. I just kind of wondered.
John Bertoni: She called me back and I said wow this I was wondering what happened. And she said thank you I think you saved my life and I said what. she said he admitted me. Her hemoglobin was so low she had to get a transfusion night. So I’m thinking well you know how it is if you gradually get more and more anemic and you learn to adapt to it. But if you go from you know a normal hemoglobin to where she was you know you wouldn’t be able to handle it right away. So she was very grateful and I said were there ever figure out why you lost blood and they had done a workup and figured that out. Nothing major league. And I said Well I do appreciate the feedback. I just kind of wondered.
Danish Bhatti: I have two questions in my mind. The first is that what drives you. You weren’t there to have your own CPR evolution done. You’re preoccupied. I know how upset I get when I have to take a (exam) and I just want to be done with it. I actually don’t want to do it and just get a certificate and you know I think I should already know all of this having done it for so long. And so you’re preoccupied you’re going there out of your schedule you have ten things to do later on. You still are on observing all of that and following up on it and taking it up and asking being the good Samaritan that nobody wants to be even in a traffic accident anymore. And then second question is that why do you still remember this. Why do you think it was such an important episode. It’s not even your patient but you want to bring it up and share it with our listeners.
John Bertoni: I don’t know the quick answer to that other than it just seemed like a good idea at the time. I guess I like questions to solve. I like to do Sudoku puzzles. I like to figure out analyze things and come up with an answer especially when it comes to medicine especially when it comes to neurology. Because if you’re observant you can learn what to ask otherwise somebody comes in or you see something on a test. This is the patient. He’s so this is his age. This was his occupation. He’s complaining of a sore leg. But if he’s in front of you you notice things. You notice lateral eyebrow here. If that’s missing it could be a thyroid problem. All these things that you know the character Sherlock — it was written and made up by a doctor. And there was a Sir Charles Bell that was a great diagnostician. He could find little things that were different. For example he could tell by where there wasn’t a tan on a guy’s forehead that he must have just gotten back from being in the British army in India. And he knew he was an enlisted man because they wore their hats a certain way in let’s say the right or the left corner of the forehead was not exposed to sun. He noticed and he said you’re just back from India.
Danish Bhatti: Now this is Sir Charles Bell.
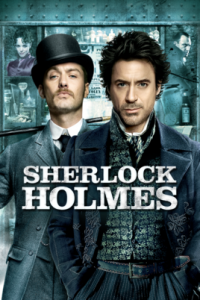 John Bertoni: Charles Bell and he was so impressed with this man’s ability to take little clues and figure things out that he just invented this character Sherlock Holmes.
John Bertoni: Charles Bell and he was so impressed with this man’s ability to take little clues and figure things out that he just invented this character Sherlock Holmes.
Danish Bhatti: Who was he impressed with?
John Bertoni: A Dr. Charles Bell who was.
Danish Bhatti: So Arthur was also a physician.
John Bertoni: Sir Arthur conan doyle was a medical student. I can’t remember if it was Edinburgh or some other English school. So we’re all that way you know when you see somebody you get a video from Pakistan you’re looking for things you see some things that are not right and you start looking for other things and then you notice there is Ataxia and there is a dystonia too or there’s a little head tilt and all of a sudden you’re going down a path and you’re collecting false positives fault you know a true positives to negatives that are really meaningful. That’s what we do for a living. And I just find it beyond that the intellectual challenges. I think if you can give someone back their health then you can say you’re cured. Go on back to your own life and I hope you find meaning in your life. But I’ve at least let you go struggle with the big questions what is my. I don’t know best calling that I can follow or what should I do with my life. How do I make it worthwhile. That’s your problem. Those are bigger questions. I’m just letting you have the freedom.
Danish Bhatti: So why bring this up?
John Bertoni: Why bring it up now?
Danish Bhatti: Yeah.
John Bertoni: Because I think there’s an important lesson for all of us in that if someone is there in front of you or a patient is their seeing you for a headache and you don’t notice the atrophy in one arm and you don’t notice that there is a lack of reflexes in the right arm and there’s something wrong with the cervical spine. And that’s the cause of the headaches that are posterior and not migraine like if you can’t put all that together by looking at things then you’re going to run up a big bill. Thinking of all the possibilities when you could zero in and figure it out and send them for a C.T. scan that the MRI scan of the neck and solve the problem. And if something is needed you know you can send them to the appropriate specialist. I don’t know. I just think that if we don’t keep our minds open to possibilities and realized it could be more than one thing when I really appreciate is I think to give quality of care you got to see past the obvious. You’ve got to say OK they’re elderly. They don’t have a sense of smell. They have Parkinson’s they’re feeble because they’re not active then are they new. Are they getting all the nutrition they should or do they have enough protein. Do they have enough iron to they have bone density that’s adequate. Can I encourage them to be more active and you know like for this Parkinson’s disease symposium just saw a lady that said Parkinson’s for 27 years and — one of our residents really interested in movement disorders is with me. And I said — this is one of those people that actually did what I asked her to do. She has a personal trainer. She has to take 15 sinemet pills a day. She’s got dyskinesia as she’s early onset. So she has dyskinesia as she’s probably near 60 but she looks normal 60 to 70 percent of the time. Functions normally takes really good care of herself is thin and very strong so that I just enjoy that one.