Alternative Therapies include herbal and nutritional supplements, exercise and massage techniques. A strong evidence for their benefit is lacking in general. Patients with Parkinson Disease (PD) routinely come across them and as many as 40% end up trying one of them. Here we will very briefly summarize the available scientific support for them, if any.
Acupuncture, is an ancient Chinese technique based on idea of stimulating energy centers in body through needles. Although several small clinical trials reported modest benefit, a meta-analysis of all combined found them no better than placebo. Some functional studies of brain have shown effects on brain; but if it translates to a clinical improvement, is not clear. The current evidence favors a placebo response.
Exercise techniques from old cultures like Tai Chi, Qigong (predecessor of tai chi and is more meditative) and Yoga have all shown some benefits in small studies. Tai Chi, the best studied, showed significant improvement in motor performance with fewer falls, compared to regular exercise.
Similarly different massage techniques (including reflexology, Trager therapy) in small studies showed improvement in Quality of Life and patient report of function. Another technique using Vibration for therapy may also be helpful, at least as a placebo. Music therapy including dancing and stepping on rhythmic cues have shown to be helpful with walking and balance.
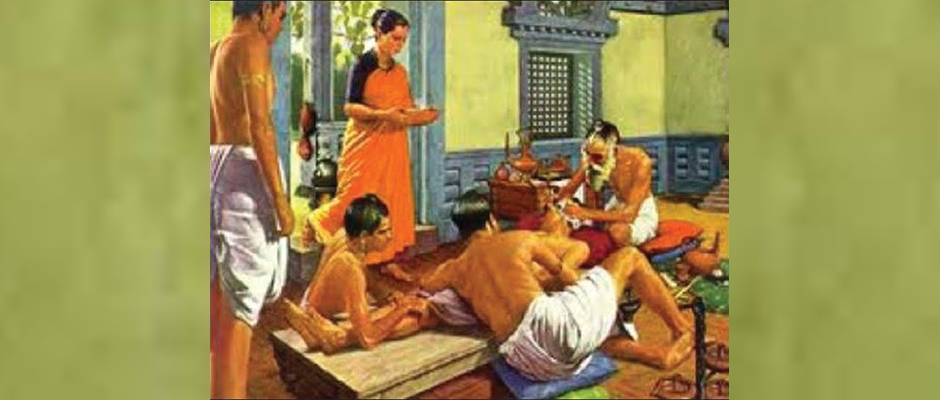
Use of Herbal supplements is more complicated. Most commonly used supplements of Velvet beans (mucuna puriens), and Broad beans (Vicia faba) are known to health care providers since ancient times. These beans mainly have Levo-DOPA (the most common and effective medical treatment for Parkinson disease) and it was originally extracted from its herbal source. These herbal extracts have shown to be similar in activity to pharmaceutical preparation. Any added advantage is not fully clear. One small study did show mucuna preparation being quicker in onset and longer lasting. However, there are no reliable suppliers of mucuna, and some suppliers tested had no mucuna/levodopa in the capsule. Some other compounds may be present in herbal extracts but their role is not clear; however similarities to other known pharmaceutical drugs in their mechanism of action have been noted.
Many other herbal and nutritional supplements have either never been studied in PD (such as Ginkgo biloba), or have outright failed to show benefit in Large well designed clinical studies (such as Co-Q10 and Vitamin E).
Role of Cannabis is even more complicated to understand. It is clear that Smoking cannabis has same cancer risks as smoking tobacco and oral formulation would be preferable, if found to be helpful. Cannabis receptors are present in the part of brain affected by PD. However their role may be mixed in reducing tremors but worsening slowness or vice versa. Added to this is the fact that there are over 60 psychoactive compounds in cannabis including both, ones that activate and others that inhibit the receptor. Further complicating the matter is that the type and quantity of chemicals differ between strains of Cannabis plant. There are small clinical studies suggesting improvement in motor features and larger trials with purified chemical extract from cannabis are underway.
To summarize, some alternative therapies have no significant added risk. Thus even though they may have only placebo benefits are worth trying. Others (like Tai Chi) are clearly beneficial. While many herbal/nutritional products are either clearly not beneficial (Co-Q10, Vitamin E) or potentially harmful in their current state of use (Mucuna, Cannabis).
Detailed Highlights:
- At least 40% PD patients use Alternate Therapies
- Acupuncture: – several clinical trials reported modest benefit. – meta-analysis of RCT found no statistical difference from Placebo.
- Bee venom: – compared with acupuncture and no treatment: greater motor benefit with bee venom, better depression control with aucupuncture,
- Tai Chi: – Randomized study comparing Tai Chi, resistance training and stretching for 24 weeks: tai chi group significant better in motor scores, fewer falls, better retention at 3 months. – small study showed better quality of life and mood with tai chi.
- Yoga: – several case reports of benefits of yoga in PD – one small randomized pilot study comparing patients regularly practicing specific yoga regimen with control shows improved motor function, posture, balance.
- Qigong: (predecessor to tai chi in traditional Chinese, focuses more on meditation then physical movement) – RCT performed found slight improvement in motor symptoms but less effective than routine exercises. No benefit on non-motor symptoms.
- Mucuna Puriens (velvet bean): – Ayurveda, the oldest document of traditional indian medicine describes its use. – 4-6% levodopa – RCT double blind by Katzenschlager, comparing Mucuna with sinemet (8 PD with motor fluctuations). Showed that mucuna has faster onset, longer period of “on time” – Animal model: neuroprotective, less dyskinesias when compared with same dose Sinemet. – No reliable supplier of mucuna, some suppliers tested had NO mucuna/levodopa in the capsule.
- Vicia faba (broad bean):
– also reported in Ayurveda, high concentration of levodopa. – One Small case series report strongly dopaminergic including dyskinesias.
– a study compared the beans vs sinemet on single dose and found slow absorption, lower peak and longer duration of beans based levodopa. No added benefit was noted. - Baanisteriopsis Caapi – another ayurvedic treatment. contains harmine and harmaline. – both compounds shown to be MAO Inhibitors. but no human studies.
- Ginkgo biloba – animal studies showing neuroprotection (MPTP models). – No PD studies.
- Co-Q 10: – large NIH trial stopped due to futility (inability to show benefit even if the trial was completed).
- Glutathione: – Small RCT showed no benefit of IV glutathione.
- Vitamin E: – No benefit (DATATOP study)
- Coconut oil and others: No data available.
- Cannabis: – Smoking cannabis has same risks as smoking tobacco and oral formulation would be preferable. – Cannabinoid Receptor CB1 is highly expressed in basal ganglia and has inhibitory effect on dopaminergic pathway. Thus agonist may potentially reduce tremor and dyskinesias while antagonist may improve akinesia. – There are over 60 psychoactive compounds in cannabis including CB1 agonists and antagonists. The type and quantity differs between strains of Cannabis plant. – animal study of agonist (THC and Cannabidiol) showed reduced dopamine depletion. – Antagonist Tetra Hydro cannabivarin is under study. – Survey in Czech reported 25% with PD responders have used it and 45% of user reported benefits. – Pilot trial showed significant improvement in motor symptoms and PD related pain 30 min. after smoking.
- Mindfulness: – mindfulness shown improved coping of PD patients. – 8 weeks of Mindfulness based program improves brain grey matter (cuneus and lingual gyrus on left) – RCT on mindfulness based life style program is under way in Australia.
- Massage: – small pilot study of whole body therapeutic massage in PD showed improvement in QOL and self-reported function. – Reflexology (massage based therapy) showed improvement in non-motor symptoms. – Träger therapy (massage based therapy) showed improved evoked stretch response in rigid limbs in PD. – Small RCT showed reduced salivary cortisol levels in PD right after treatment.
- Alexander Technique: (improving posture through feedback) – Small (underpowered) study comparing alexander technique with massage and no treatment. Both
– interventions were better for self-reported symptoms and depression but not any different between each - Vibration Therapy: – J M Charcot first noticed patient feeling better after train and carriage rides and first tried vibration therapy. – Several studies with whole-body vibration showed improvement in motor symptoms. – Two recent studies used placebo groups with partial blindness and showed no significant improvement over placebo.
- Music Therapy: – A meta-analysis of several music based movement trials showed benefit on several balance measures. – Tango based dance therapy showed positive effect on gait and balance. – Likely involvement of reward system pathway (dopaminergic) – Several trials showed benefit of rhythmic cuing on gait speed, step length and freezing of gait.